PRODUCT
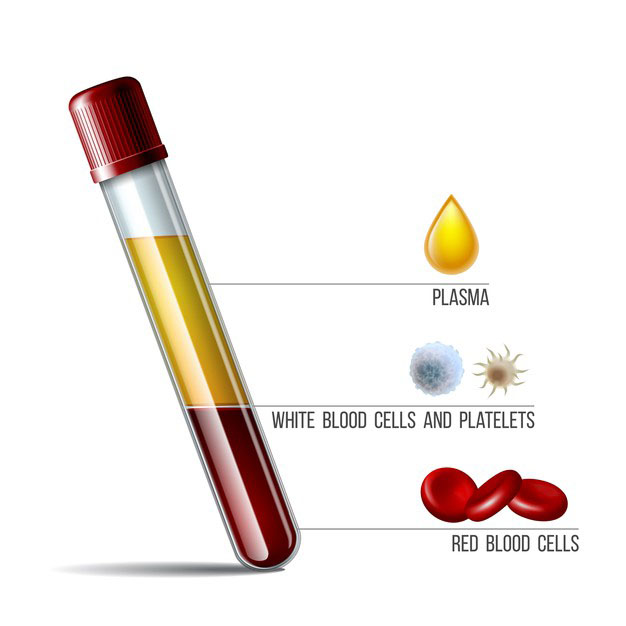
The collected blood is getting separated in the following components
- Packed Red Blood Cells-PRBC
- Random Donor Platelets-RDP
- Fresh Frozen Plasma-FFP
- Cryo Poor Plasma-CPP
- Single Donor Platelets -SDP
- Covid Convalescent Plasma -CCP
Packed Red Blood Cells-PRBC
- In Severe anemia, Hemoglobin % is lower 5gms: as per treating doctor's diagnosis.
- In a Patient generally One Unit of Blood Transfusion Increases Hb % by 1 gm % in a person with 60 Kg Weight( with No active Bleeding )
- In Thalassemia (Genetic defect Alfa &/or Beta Chains): RBCs have short life span so for patients' survival and healthy life continuous repeated Blood Transfusions are needed.
- In Sickle cell anemia: Genetic Defect: RBCs have Fetal Hemoglobin & form Soccer shape at high altitude, Due to RBC shape is destroyed in spleen rapidly causing anemia.
- During Operative Procedures There is Blood loss and at times its more than one unit of Blood Here as a replacement therapy & for maintaining Oxygen levels & some times in Moderate to severe Blood loss Massive Blood Transfusions may be required to save the Patients.
- Pregnant Ladies during delivery, Caesarian section & Post Partum can be major Blood loss threatening life. Occasionally atone of Uterus can lead to severe Blood loss and needs urgent Blood Transfusion as Life saving treatment.
- Any Road Accident or accident leading to Blood Loss. Accident with Blood loss of 2 Units of Blood & or Hemoglobin less than 10 gms with reducing Hb, Abnormal Vital signs and moderate to severe injury will need Emergency Blood Transfusion as the Life Saving requirement.
- Exchange Transfusion: Whole Blood / PCV along with Plasma is used for exchange transfusion in New Born Babies in Hemolytic Disease due to Rh incompatibility.
- In Major Operations like Organ Transplant / Cardiac Surgery.
Platelets: Use As Life Saver
- Platelets are tiny blood cells that help your body form clots to stop bleeding.
- If one of your blood vessels gets damaged, it sends out signals to the platelets. The platelets then rush to the site of damage; they form a plug (clot) to fix the damage.
- Clinical conditions with platelet count at warning level: depends upon the clinical diagnosis and concerned operative procedures.
- The process of spreading across the surface of a damaged blood vessel to stop bleeding is called adhesion.
- This is because when platelets get to the site of the injury, they grow sticky tentacles that help them stick (adhere) to one another.
- They also send out chemical signals to attract more platelets. The additional platelets pile onto the clot in a process called aggregation.
- Platelet transfusion, also known as platelet concentrate, is used to prevent or treat bleeding in people with either a low platelet count or poor platelet function. Often this occurs in people receiving cancer chemotherapy.
- One unit of Random Donor Platelets (50-70 ml) increases Platelet count by 5000-6000 platelets While Single Donor Platelets (220-250 ml) increases platelet count by 50,000-60,000 /cmm.
- Viral Fever e.g. Dengue,
- D.I.C. (Small Blood clots in Blood Vessels): Platelet consumption & destruction leads to low Platelet count which may lead to Bleeding.
- Cancer Patients on Treatment.
- Blood group matching (ABO Rh system) is typically recommended before platelets are given.
- Unmatched platelets, however, are often used due to the unavailability of matched platelets. They are given by injection into a vein.
Fresh Frozen Plasma: Provides Clotting Factors
- Fresh Frozen Plasma is indicated for the deficiency of coagulation factors with abnormal coagulation tests in the presence of active bleeding.
- FFP is also indicated for a planned surgery or invasive procedure in the presence of abnormal coagulation tests, for the reversal of Warfarin in the presence of active bleeding or planned procedure when vitamin K is inadequate to reverse the Warfarin effect, thrombotic thrombocytopenic purpura, and congenital or acquired factor deficiency with no alternative therapy.
- Other more specific recommendations for FFP based on systematic review include trauma patients requiring massive transfusion and warfarin-related intracranial hemorrhage.
- Other situations where the administration of FFP cannot be recommended for or against based on systematic review include FFP transfusion at a plasma-to-RBC ratio of 1:3 or more in trauma patients with massive transfusion.
- Genetic abnormality lacking one or more Clotting Factors may bleed with precipitating cause and FFP is needed as Life saving treatment.
- In Some Autoimmune diseases: Auto antibodies are developed which cannot identify its own body tissue of Host: Here Plasma Exchange Therapy works as Magic treatment.
- In Recent Covid -19 out Break: Plasma from Recovered Covid-19 patients is used to treat Moderate to severely ill Covid -19 Patients to fasten the recovery –Recovery varies from patient to patient.
Cryoprecipitate : Use
- Cryo is prepared from FFP.
- Volume is 15-20 ml.
- In cardiac Patients as well as in Children It is used for Coagulation Factors as with less quantity of blood Component will supply the Coagulation Factors.